Glossopharyngeal neuralgia (GPN) is a rare yet debilitating condition characterized by sudden, sharp, and stabbing pain in areas innervated by the glossopharyngeal nerve (cranial nerve IX), including the throat, base of the tongue, tonsils, and ear. This pain can significantly impair quality of life, leading patients to avoid eating, talking, or even swallowing. In severe cases, glossopharyngeal neuralgia may also involve the vagus nerve (cranial nerve X), resulting in additional symptoms such as bradycardia, syncope, and laryngeal discomfort. This combined condition is often referred to as vagoglossopharyngeal neuralgia, and its management can be particularly complex.
Understanding the Surgical Strategy
When medication (such as carbamazepine or gabapentin) fails to control the pain or causes intolerable side effects, surgical intervention becomes necessary. One surgical strategy involves sectioning (cutting) the vagoglossopharyngeal complex, which includes both the glossopharyngeal and vagus nerves, to interrupt the pain signals at their source.
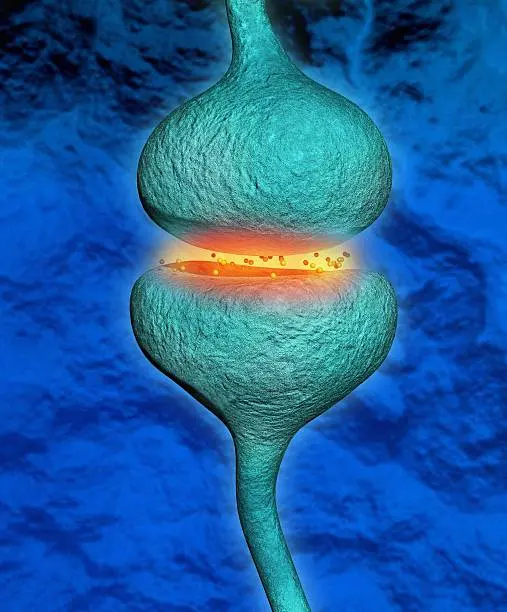
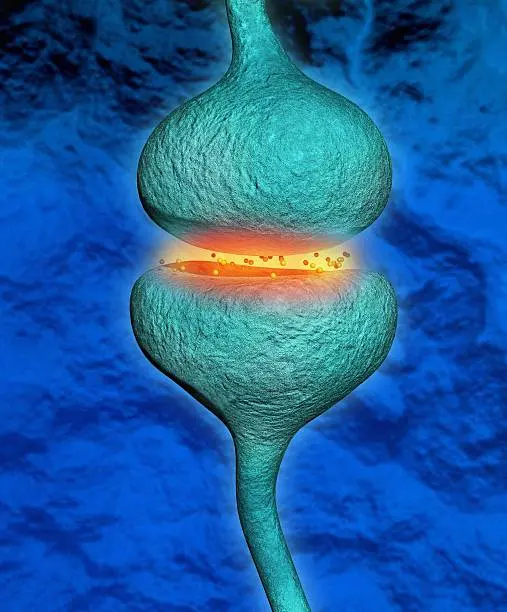
An alternative or adjunctive approach is microvascular decompression (MVD). This procedure involves identifying and relieving pressure from an artery (often the posterior inferior cerebellar artery, or PICA) that may be compressing the nerve at its root entry zone in the brainstem. Compression from such vessels is thought to cause abnormal nerve firing and chronic pain. By decompressing the nerve, normal function and pain-free status can often be restored without destroying the nerve itself.

With or Without Decompression: What Are the Outcomes?

The main question in the surgical management of GPN is whether nerve sectioning alone is sufficient, or whether combining it with microvascular decompression offers better long-term outcomes especially in terms of pain-free survival and preservation of neurological function.
Clinical studies and surgical case series have shown promising results for both approaches

How Do We Measure “Pain-Free Survival”?
“Pain-free survival” refers to the duration of time after surgery during which the patient remains free of glossopharyngeal neuralgia symptoms without the need for medications. Long-term follow-up studies indicate that both sectioning and MVD can lead to excellent outcomes:
Sectioning without MVD
Pain relief is often immediate and durable, with success rates between 80% and 90%. Some mild sensory or vocal changes are common but generally well tolerated.